GILROY—Dozens of workers at Saint Louise Regional Hospital, from its chief of staff to its nurses, along with citizens and elected officials spoke of the need to keep the Gilroy hospital open at a hearing hosted by the California Attorney General’s Office. The Oct. 16 session at Gilroy City Hall was one of a handful held in California as Attorney General Kamala Harris reviews the proposed sale of Saint Louise and five other hospitals to New York-based private equity firm BlueMountain.
Many urged Harris to impose conditions on the transaction that would protect essential services for the poor and sick over the next decade.
“The Attorney General’s Office holds the future of Saint Louise Regional Hospital in her hands,” said Saint Louise CEO Sister Margaret Keaveney, who replaced Jim Dover in May. Harris has 105 days to review and consider approval of the transaction, which was initiated July 31.
But hospital administrators tempered calls ensuring certain services do not disappear with pleas to sidestep “unreasonable conditions” that could lead to continued turmoil.
A hearing in January hosted by the Attorney General’s Office on the then-proposed sale to Ontario-based Prime Healthcare drew hundreds of people to Gilroy, including two separate crowds from opposing unions that supported different prospective buyers. Prime ultimately walked away from the $843 million deal. Its executives said Harris’ long-term conditions requiring the system to retain many services for at least 10 years were too much to bear.
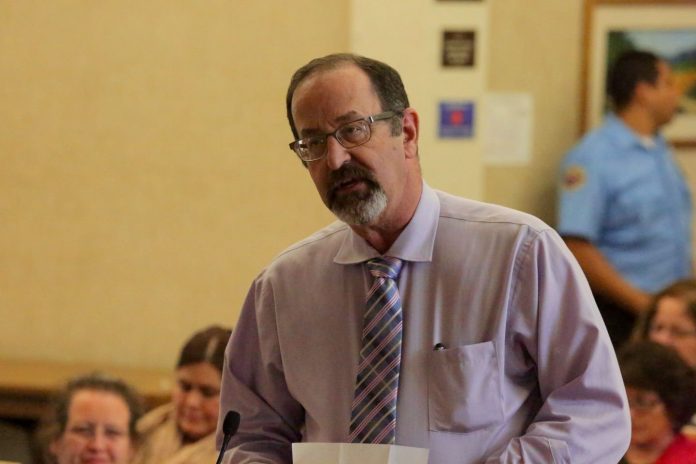
Dr. Jack Fisher, chief of staff at Saint Louise and a Gilroy-based podiatrist for 41 years, spoke of the urgent need to turn the page in this chapter of the hospital’s history at the hearing, attended by approximately 100 people.
“The doctors and associates at our hospital are doing an outstanding job of caring for our patients in spite of the cloud of uncertainty that hangs over our heads on a daily basis,” Fisher said. “We are frustrated; we are tired and we are just plain worn out due to the prolonged process of finding a new owner.”
Fisher and other Daughters of Charity officials said they are encouraged by the vision of BlueMountain and are confident they can succeed—if the deal is approved and the conditions are reasonable.
Under the terms of the proposed agreement, a management team through Integrity Healthcare LLC, a newly formed company, will oversee hospital operations for at least 15 years, replacing the Daughters of Charity’s existing board of directors.
The Daughters of Charity Health System will be called Verity Health System, and BlueMountain and Integrity Healthcare have agreed to inject $160 million for “turnaround efforts,” from capital improvement projects to expanding a team of doctors, according to the agreement. Verity will not have a religious affiliation like the Catholic-affiliated Daughters of Charity. After three years, and the attorney general’s approval, BlueMountain will have the option to convert Verity into a for-profit health system from its current nonprofit status.
Deputy Attorney General Wendi Horwitz, Harris’ representative Oct. 16, said all parties have agreed to continue operating the facilities as general acute-care hospitals with open emergency departments “subject to physician availability, the needs of the community and the financial viability of such services.”
Integrity also agreed, for at least five years from the close of the transaction, to continue existing charity care policies for the indigent or replace them with policies “of either similar or greater benefit to the community,” according to Horwitz.
As a result, BlueMountain managing partner Peter Greatrex said the system would be on much stronger financial footing.
“The capital will, with a strong focus on operational improvement, stabilize the struggling hospital system,” he said.
However, whether certain services continue for five, 10 or even 50 years was a hot topic at the hearing.
Many urged Harris to implement long-term conditions on the transaction to ensure emergency medical services and other essential programs continue at least at existing levels for a decade. That includes a healthcare consultant contracted with the Attorney General’s Office to analyze the potential local impacts on the proposed sale.
Phil Dalton, president of Medical Development Specialists, LLC, presented a report detailing the conditions he recommends if the attorney general approves the deal.
For at least 10 years from the closing date, the report says Harris should require protection of existing emergency medical services, obstetrics, intensive care beds, stroke services and others. The conditions are recommended “to minimize any potential negative health impact that might result from the transaction,” Dalton said.
The report also recommends Morgan Hill’s DePaul Urgent Care Center, a Daughters facility, remain open and available to patients seven days a week for at least five years.
Peggy Elwell, who missed a hearing on O’Connor Hospital in San Jose the morning of Oct. 16 and drove to Gilroy to give her two cents, urged Harris to “extend those conditions [protecting current services and employees] as long as possible.”
“It seems like we’re faced with no good choices,” she said, wondering aloud what caused this situation of no assurances.
Gilroy Councilman Perry Woodward said the proposed conditions appear to be “onerous” and could threaten the survival of the local hospital.
“This seems to me the clearest path to keeping a hospital in South County,” Woodward said of the deal currently under review. “If this doesn’t work—if the hospital goes bankrupt—I don’t see it working out. We’d like to avoid that as a community.”
In order for the hospital system to be successful, flexibility regarding the services its hospitals offer and the contracts it maintains is vital, added Saint Louise vice president of clinical services Lori Katterhagen.
“We are ripe and ready for change. But to put unreasonable conditions on the transfer of this hospital system would be a grave injustice done by the attorney general’s office,” she said. “We need to be able to maneuver and adapt to the growing needs of this community.”
Registered nurse Christine Dixon said she can’t imagine the impact of the loss of the Gilroy hospital, which would require patients drive upwards of 30 miles to the nearest hospital. In order to continue services at existing levels and caring for the underserved, Dixon asked Harris to include conditions that preserve jobs, labor contracts, pensions and a safe working environment.
Vice-chair of the SLRH board of directors Alan Hayes said it’s not appropriate to impose 10-year conditions in this current healthcare environment.
“With the continued turmoil we’ve experienced since the mid-1980s, to look 10 years down the road and demand certain conditions today that might not be viable 10 years from now…is not fair or doable.”













