Q: I heard that women with endometriosis are more likely to have
other medical problems, including ovarian cancer. What can I do to
lower my risk?
By the Faculty of Harvard Medical School
Q: I heard that women with endometriosis are more likely to have other medical problems, including ovarian cancer. What can I do to lower my risk?
A: “Killer cramps” is how many women with endometriosis describe the worst symptom of this disease, which affects up to 1 in 10 women. Women with endometriosis are slightly more likely to develop ovarian cancer than those without the disease. The reassuring news is that ovarian cancer is rare, and the increased risk is quite small. And a widely used treatment for endometriosis helps minimize the risk.
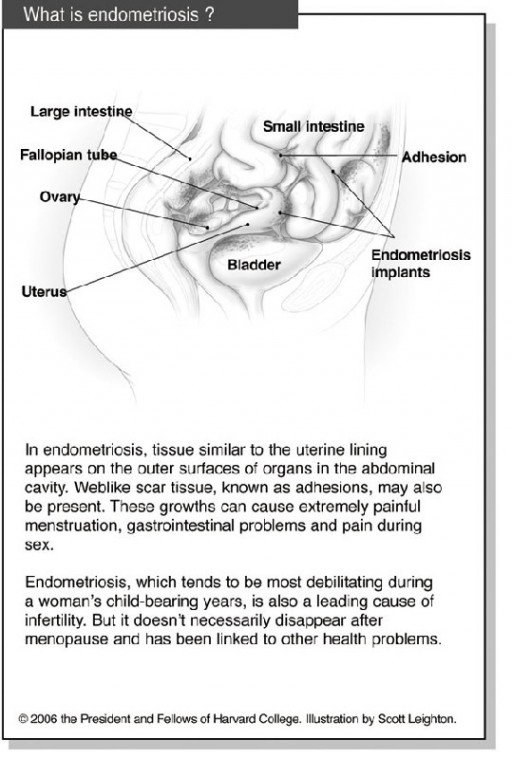
Endometriosis occurs when tissue similar to the inside lining of the uterus shows up where it shouldn’t – on the outer surfaces of the uterus, on the walls of the abdominal cavity and on the ovaries, fallopian tubes and nearby organs (see graphic). This wayward tissue builds up and sheds monthly in response to the menstrual cycle. But unlike menstrual fluid, which exits through the vagina, the blood and tissue remain trapped in the body. This triggers swelling and web-like scar tissue that binds organs together, known as adhesions. Experts estimate that among women with pelvic pain, infertility or both, up to half have endometriosis.
Treatments include surgery to remove the misplaced tissue and drugs that suppress or regulate menstruation. Many women say that they get some relief from dietary changes (avoiding red meat, caffeine, alcohol, and refined flour and sugar). Acupuncture, massage, and relaxation techniques such as yoga or meditation, may also help. But these approaches are not proven for treating endometriosis.
It’s not clear why women with endometriosis are slightly more likely to develop ovarian cancer. But taking birth control pills – a common treatment for endometriosis – for five years or more can cut ovarian cancer risk by as much as 40 percent.
Ovarian cancer can mimic endometriosis. The symptoms include abdominal pain, swelling, fatigue, back pain and a frequent need to urinate. Women who have had endometriosis should be alert to this possibility, especially if symptoms recur after menopause, when most ovarian cancers develop. Several reports also suggest a link between endometriosis and a higher risk for breast cancer, non-Hodgkin’s lymphoma and melanoma.
If you have endometriosis, be sure to have annual checkups and any tests recommended by your clinician.
Women with severe symptoms who’ve gotten no relief from various medical and surgical treatments often resort to hysterectomy – sometimes in their 30s or 40s, or even earlier. Most also have their ovaries removed, which results in “surgical menopause.” Even then, endometriosis may persist if tiny bits of ovarian tissue remain in the pelvis.
A recent study suggests that removing the ovaries before age 65 has a downside. It may increase the risk of heart disease and osteoporosis, which are far more common than ovarian cancer. This is one reason why doctors say that ovary removal should be decided on a case-by-case basis. Most experts agree that women with endometriosis who undergo surgical menopause should probably take hormone therapy until natural menopause (around age 51).
Medications that lower estrogen levels to suppress endometriosis may also raise a woman’s risk for osteoporosis. These medications, called GnRH agonists (Lupron, Synarel, Zoladex and others), stop a woman’s periods, creating a temporary menopause. This eases endometriosis symptoms but may also weaken bones. Women who take these medications may be given small amounts of other drugs to prevent bone loss. They also should be diligent about bone-density testing and bone-healthy habits, and follow-up with their clinicians.
There’s also evidence that women with endometriosis have a higher-than-average risk of autoimmune and related disorders. Researchers have found that, compared with American women in general, women who had endometriosis were 100 times more likely to have chronic fatigue syndrome, seven times more likely to have hypothyroidism and twice as likely to have fibromyalgia. Multiple sclerosis, rheumatoid arthritis, lupus, Sjogren’s syndrome, allergies, and asthma were also more common. Women who have endometriosis should be alert to any new symptoms that could signal one of these conditions.
Submit questions to the Harvard Medical School Adviser at www.health.harvard.edu/adviser. Unfortunately, personal responses are not possible.